If you’re waking up to sharp heel pain or you struggle with discomfort after long periods on your feet, you might be experiencing symptoms of plantar fasciitis. This common condition is more than just a nuisance; it’s the inflammation of your plantar fascia, the thick band of tissue that runs across the bottom of your foot connecting your heel bone to your toes. It can make routine activities challenging and hinder your mobility, but the good news is, with the right approach, it’s manageable.
Enter physiotherapy, a powerful tool in your arsenal against this persistent heel pain. Physiotherapists can offer a range of treatments tailored to reduce your discomfort, improve foot function, and get you back on your feet—literally. Through stretches that elongate the plantar fascia, strengthening exercises for lower leg muscles, and techniques like athletic taping, physiotherapy addresses both the symptoms and the underlying causes of plantar fasciitis.
Living with heel pain can be discouraging, but you don’t have to accept it as your new normal. If you’re in/around Vancouver and looking for a solution, consider paying a visit to Reformotiv.
What is Plantar Fasciitis
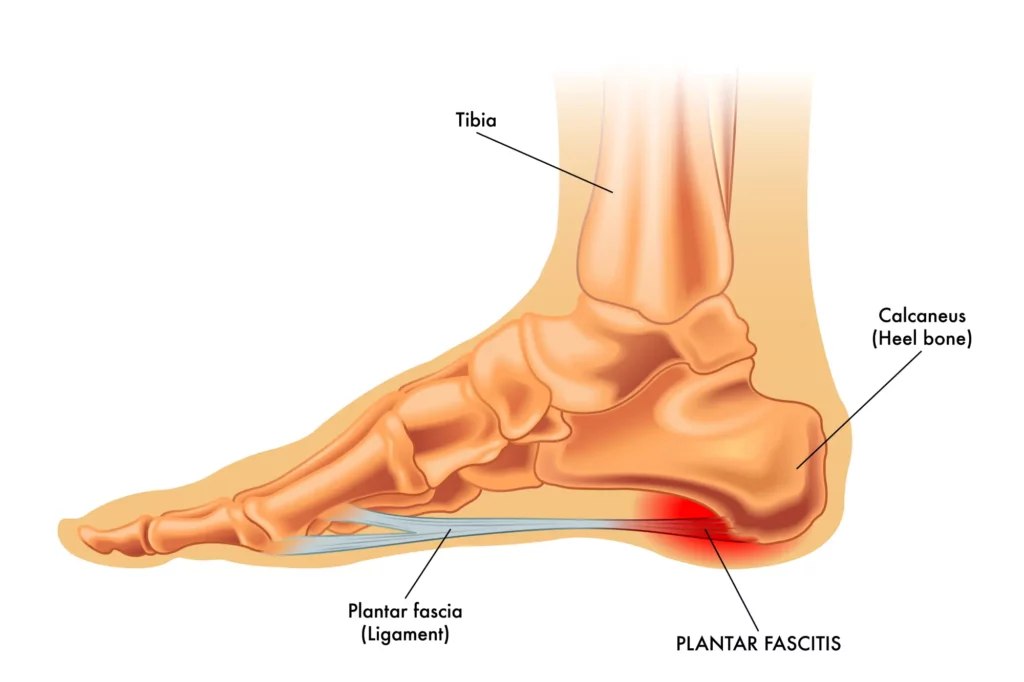
Plantar fasciitis is the inflammation of the plantar fascia, a band of tissue that connects your heel to your toes, and it’s a common source of heel pain. This condition typically causes discomfort at the bottom of your foot, particularly after periods of inactivity (i.e. first few steps out of bed in the morning) or vigorous activity.
Anatomy of the Plantar Fascia
The plantar fascia is crucial for foot biomechanics, supporting the arch and absorbing shocks as you walk. When it’s strained, microscopic tears can develop, leading to inflammation and resulting in heel pain and tenderness.
Understanding the anatomy and etiology of plantar fasciitis can help pinpoint effective treatments like physiotherapy to reduce symptoms and improve foot function. If you have persistent heel pain, it’s vital to consider your activity level, muscle imbalances, any chronic conditions, or excess body weight as potential contributing factors.
Symptoms of Plantar Fasciitis
When dealing with plantar fasciitis, your first signal is often a sharp pain in the heel. This pain is typically most intense with the first steps that you take in the morning or after a period of rest. As you move about, the pain usually decreases, but it might return after long periods of standing or when you stand up after sitting.
You may notice that the heel pain is worse when you’re climbing stairs or after standing for an extended time. The discomfort can become a dull ache that can persist throughout the day.
Here’s a simplified list of common symptoms that you might experience if you have plantar fasciitis:
- Sharp pain in the heel
- Stiffness in the heel area
- Ache that extends through the heel
- Increased discomfort after rest, decreasing then returning after activity
It’s critical to pay attention to these symptoms, as they can guide you in seeking appropriate physiotherapy treatment and managing the condition effectively.
Remember, your experience with plantar fasciitis may vary, and not everyone will have the same symptoms. If your pain doesn’t improve, or you have concerns, consider consulting a healthcare professional to explore the full range of therapeutic options available to you.
Causes of Plantar Fasciitis
You might wonder why your heel hurts when you take those first steps in the morning. The culprit could be plantar fasciitis, and understanding its causes is the first step towards managing the pain. Here are some potential causes that strain and stress the plantar fascia:
- Repetitive Stress: Activities that place a lot of stress on your heel and attached tissue — like long-distance running, ballistic jumping, or ballet dancing — can contribute significantly. Sometimes it can be a matter of jumping into an activity without proper warm-up or ramping up the load/intensity too quickly that causes your tissue to get irritated.
- Biomechanics: Your foot mechanics can be the key. Flat feet, a high arch, or even abnormal walking patterns can affect the way weight is distributed when you’re standing/walking and can put added stress on the plantar fascia.
- Imbalances up the chain: Old injuries, habits, muscle imbalances, stiff joints, and more can all lead to altered loading through the body. Your body is great at adapting to keep you functional but sometimes it runs out of options and that one pattern can lead to overloading along the chain. Plantar fasciitis can result when the feet have had to adapt to take more load from the knees, hips, or pelvis.
- Occupation: If your job has you on your feet on hard surfaces for long hours, it may set the stage for plantar fasciitis. Think teachers, healthcare workers, factory workers, or restaurant staff.
- Weight: Extra pounds can put extra stress on your plantar fascia, so maintaining a healthy weight might help you avoid the pain associated with plantar fasciitis.
- Improper Footwear: Shoes that don’t support your type of arch or provide enough cushion can lead to plantar fasciitis.
Understanding these factors is key—after all, your feet get you where you need to go. So, give them the attention they deserve and keep an eye out for these potential root causes of plantar fasciitis.
Physiotherapy Approaches
In addressing plantar fasciitis, physiotherapy plays a pivotal role in both managing pain and promoting healing. By employing a range of techniques from initial pain management to more advanced therapies, physiotherapy can significantly improve your foot function and relieve discomfort. As no one treatment approach is the same, the key to effective recovery will be a thorough assessment of your movement patterns, lifestyle contributions, footwear, strength, and overall function.

Initial Pain Management Techniques
To kickstart your recovery journey, initial pain management is crucial. You’ll likely start with ice application to reduce inflammation. Your physiotherapist may also recommend night splints to gently stretch your calf muscles and the arch of your foot while you sleep. This ensures a reduction in morning pain typically associated with plantar fasciitis. Moreover, arch supports, athletic taping, or orthotics can be utilized during daily activities to alleviate pressure on the heel bone and provide better support. As well, manual therapy and soft tissue techniques are highly effective to reduce inflammation and improve joint mechanics related to the cause(s) of your plantar fasciitis.
Stretching and Strengthening Exercises
Your physiotherapist will guide you through personalized stretching exercises targeting the plantar fascia, Achilles tendon, and calf muscles—which include both the gastrocnemius and soleus. Regular mobility and stretching helps relieve tension and improve flexibility and circulation. Additionally, strengthening exercises will be introduced to bolster the muscles around your foot and ankle as well as the whole lower extremity, enhancing support and stability. Incorporating functional strengthening exercises will be important for returning to healthy and pain-free gait, stairs, sports, and daily activities.

Preventing Recurrence
Plantar fasciitis can recur if you’re not diligent with preventive measures. Below, you’ll find specific strategies and signs to watch for to keep your feet healthy.
Ongoing Management Strategies
- Exercise and Stretching: Regular, gentle exercises can strengthen your foot muscles, improving stability and reducing stress on your plantar fascia. Incorporate daily stretching of the Achilles tendon and plantar fascia to maintain flexibility.
- Arch Support: Wearing shoes with proper arch support distributes your weight more evenly during weight-bearing activities, which may prevent excessive strain.
- Weight Management: Staying at a healthy weight minimizes the pressure on your feet, which can alleviate the load your plantar fascia bears during prolonged standing or walking.
- Repetitive Strain and Prolonged Standing: Modify your activities or introduce slower increases in activity to reduce repetitive strain, and take breaks to limit time spent on your feet.
- Physical Therapy: Regular physical therapy sessions can provide you with personalized exercises and manual therapy to boost recovery and prevent future injuries.
Conclusion
Plantar fasciitis can significantly impact your daily life and mobility.
It’s essential to consult with a qualified physiotherapist who can develop a personalized and effective treatment strategy for you. Remember, persistence and adherence to your therapy program are key to overcoming plantar fasciitis.
Feel free to connect with the highly skilled team of Physiotherapists at Reformotiv in Vancouver for a comprehensive evaluation and to kickstart your journey towards pain-free feet.

